

| Transport Instructions | |||
| Collection Location | Transport Temperature | Processing Required | Timeframe |
| ED/Inpatient | Room Temperature | None | Specimen must be received by the lab within 2 hours of collection |
| Laboratory/ Outpatient/ Off-Site |
Room Temperature | Allow blood to clot for 30 minutes in a vertical position. Centrifuge to separate from cells within 2 hours of collection. | Specimen must be received by the lab within 24 hours of collection |
| Refrigerated (Ice Packs) | Allow blood to clot for 30 minutes in a vertical position. Centrifuge to separate from cells within 2 hours of collection. | Specimen must be received by the lab within 7 days of collection | |


| HSV-1 IgG Antibody Result Interpretation | |
| Result | Interpretation |
| Negative | No detectable antibodies to HSV-1 were found. A negative result generally indicates that the patient has not been infected, but does not always rule out acute HSV infection. If clinical exposure to HSV is suspected despite a negative finding, a second sample should be collected and tested no less than 4 - 6 weeks later. |
| Equivocal | Equivocal samples are retested in duplicate by the LIAISON HSV-1 assay in order to confirm the equivocal result. A second sample should be collected and tested no less than 4 - 6 weeks later when the result is confirmed as equivocal. |
| Positive | Indicates the presence of detectable IgG antibody to HSV-1. |
| HSV-2 IgG Antibody Result Interpretation | |
| Result | Interpretation |
| Negative | No detectable antibodies to HSV-2 were found. A negative result generally indicates that the patient has not been infected, but does not always rule out acute HSV infection. If clinical exposure to HSV is suspected despite a negative finding, a second sample should be collected and tested no less than 4 - 6 weeks later. |
| Equivocal | Equivocal samples are retested in duplicate by the LIAISON HSV-2 assay in order to confirm the equivocal result. A second sample should be collected and tested no less than 4 - 6 weeks later when the result is confirmed as equivocal. |
| Positive | Indicates the presence of detectable IgG antibody to HSV-2. |
| Ordering |
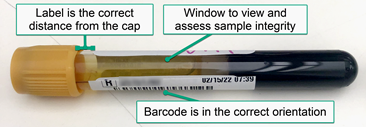
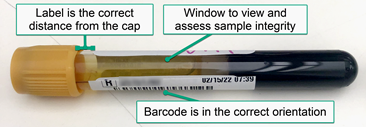
| Collection |

| Transport Instructions | |||
| Collection Location | Transport Temperature | Processing Required | Timeframe |
| ED/Inpatient | Room Temperature | None | Specimen must be received by the lab within 2 hours of collection |
| Laboratory/ Outpatient/ Off-Site |
Room Temperature | Allow blood to clot for 30 minutes in a vertical position. Centrifuge to separate from cells within 2 hours of collection. | Specimen must be received by the lab within 24 hours of collection |
| Refrigerated (Ice Packs) | Allow blood to clot for 30 minutes in a vertical position. Centrifuge to separate from cells within 2 hours of collection. | Specimen must be received by the lab within 7 days of collection | |


| Result Interpretation |
| HSV-1 IgG Antibody Result Interpretation | |
| Result | Interpretation |
| Negative | No detectable antibodies to HSV-1 were found. A negative result generally indicates that the patient has not been infected, but does not always rule out acute HSV infection. If clinical exposure to HSV is suspected despite a negative finding, a second sample should be collected and tested no less than 4 - 6 weeks later. |
| Equivocal | Equivocal samples are retested in duplicate by the LIAISON HSV-1 assay in order to confirm the equivocal result. A second sample should be collected and tested no less than 4 - 6 weeks later when the result is confirmed as equivocal. |
| Positive | Indicates the presence of detectable IgG antibody to HSV-1. |
| HSV-2 IgG Antibody Result Interpretation | |
| Result | Interpretation |
| Negative | No detectable antibodies to HSV-2 were found. A negative result generally indicates that the patient has not been infected, but does not always rule out acute HSV infection. If clinical exposure to HSV is suspected despite a negative finding, a second sample should be collected and tested no less than 4 - 6 weeks later. |
| Equivocal | Equivocal samples are retested in duplicate by the LIAISON HSV-2 assay in order to confirm the equivocal result. A second sample should be collected and tested no less than 4 - 6 weeks later when the result is confirmed as equivocal. |
| Positive | Indicates the presence of detectable IgG antibody to HSV-2. |