
Upper respiratory specimens: nasopharyngeal swab in UTM
Lower respiratory specimens: BAL, Bronch wash, ETT, TA, Sputum in sterile container. (Tested at UR Central Lab)
Specimen source is required.
Highland Hospital: NP swabs in UTM for on-site testing. All lower respiratory samples are sent to the UR Central Lab for testing.
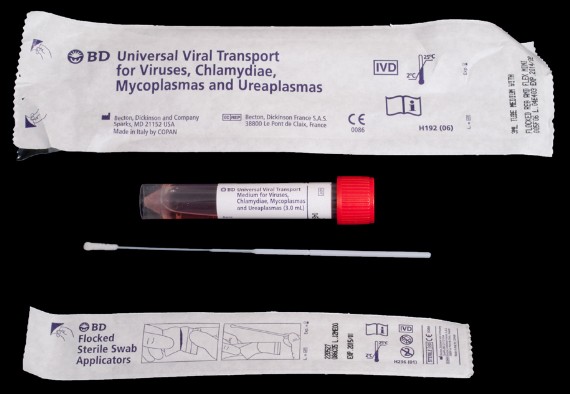
UNIVERSAL TRANSPORT MEDIA
| Result Test ID | Reportable | Result Test Name | Result Type | Type (Alpha or Numeric) | Prompt Test |
| INFA2 | Y | INFLUENZA A NAAT | I | A | N |
| INFB2 | Y | INFLUENZA B NAAT | I | A | N |
| RSVR2 | Y | RSV NAAT | I | A | N |
| SORC6 | Y | FLU/RSV SOURCE | I | A | Y |
| Specimen Requirements |
Upper respiratory specimens: nasopharyngeal swab in UTM
Lower respiratory specimens: BAL, Bronch wash, ETT, TA, Sputum in sterile container. (Tested at UR Central Lab)
Specimen source is required.
Highland Hospital: NP swabs in UTM for on-site testing. All lower respiratory samples are sent to the UR Central Lab for testing.
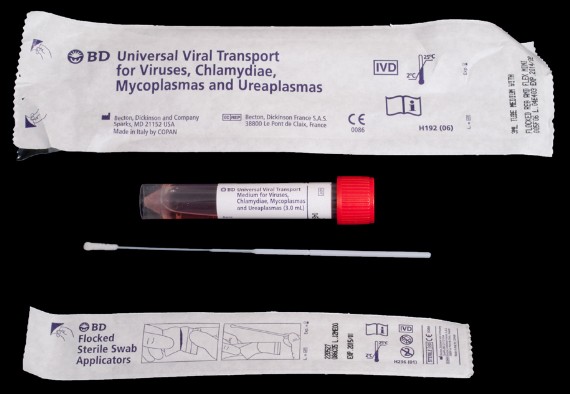
UNIVERSAL TRANSPORT MEDIA
| Testing |
| Result Interpretation |
| Coding |
| URM Labs Internal |
| Test Build |
| Result Test ID | Reportable | Result Test Name | Result Type | Type (Alpha or Numeric) | Prompt Test |
| INFA2 | Y | INFLUENZA A NAAT | I | A | N |
| INFB2 | Y | INFLUENZA B NAAT | I | A | N |
| RSVR2 | Y | RSV NAAT | I | A | N |
| SORC6 | Y | FLU/RSV SOURCE | I | A | Y |